
A fracture of the small outermost bone of a toe or finger may not only hurt, but also may contain a hidden threat that is not yet visible on plain x-ray pictures at the time of injury.
I start with a technical (medical) description of the situation: any dorsal Salter 2 fracture of a distal phalanx may lead to destructive osteomyelitis (bone infection) of that involved toe or finger.
Now to try to explain my terms:
Dorsal refers to the back of the hands and fingers or the top of the toes.
A fracture is a break in a bone.
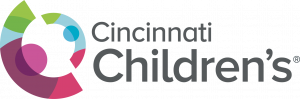
A Salter 2 fracture is a fracture that goes through the metaphysis and also the physis of a bone. The physis, or growth plate, is the cartilage allowing growth of the bone, which shows up on x-rays as a darker zone between the epiphysis at the end of the bone and the metaphysis, which is the shaft portion on the other side of the physis (see diagram 1).
A distal phalanx is the outmost bone of the bones in each finger or toe.
Such fractures are usually the result of direct injury to the finger or toe, commonly known as stubbing. Most commonly involved are the great toe and the thumb.
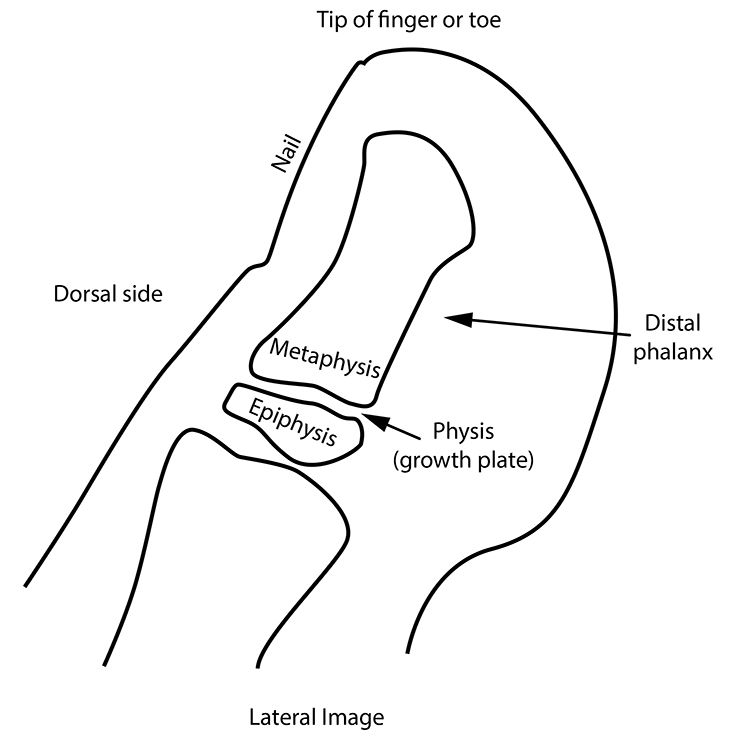
As a result, on the x-ray (as well as on physical exam) the digit shows soft tissue swelling just proximal [in the direction of the ankle or wrist] to the nail of the digit.
Because such fracture often entails a small break in the skin at the side of the nail, bacteria may gain access to the inside of the finger or toe. The nail bed is highly vascular, as is the nearby metaphysis. This means that infection could easily travel within the toe or finger to the fractured metaphysis (see diagram 2). This means an infection of the bone (known as osteomyelitis) can occur in that metaphysis.
Unfortunately for diagnosis, it takes at least 9 or 10 days for osteomyelitis to be recognizable on plain x-rays (either by bone destruction or by calcification alongside the affected bone), so that by x-ray alone, the infection is a hidden threat for a little over a week. Your doctor, if aware of the dorsal Salter 2 stubbed toe or finger fracture, may choose to give your child an antibiotic to prevent the infection or else observe the finger or toe over the next week and a half to look for clinical signs of infection. If an x-ray after 10 days does not show evidence of osteomyelitis, then the hidden threat has passed. Unfortunately, many stubbed finder or stubbed toe fractures do manifest osteomyelitis if untreated.

Be aware that it is only the lateral image (side view) that shows all the structures mentioned above that can be injured by stubbing, as on Diagram 2. It is also important not to have any finger or toe overlying the x-rayed digit.
The Salter 2 fracture fragment of the metaphysis is often quite subtle, so the zooming (enlarging) of the original lateral image is important in its detection on the original lateral x-ray.
It would also be prudent to consult a doctor or other health care professional if your child develops a fever during the 10-day hidden threat period, since osteomyelitis can certainly cause fever (as well as increased pain).
Dr. Alan E. Oestreich, author; Glenn Miñano, BFA, editor; Meredith Towbin, copyeditor
