
Photo: Nuclear medicine technologist transferring radioactive agent into container
Hepatobiliary tumors in the pediatric population represent 5-6% of abdominal tumors, and liver tumors account for 0.5-2% of cancer in children. Pediatric tumors are typically radiosensitive, but the use of necessary radiation doses via external beam radiation in young children is limited by direct liver toxicity. Selective internal radiation therapy (SIRT), or radioembolization, allows selective liver tumor irradiation and avoids the limitations of external beam radiation; it is the injection of radioactive particles into the hepatic artery (artery that supplies blood to the liver) via an artery in the groin. This allows targeted treatment in patients with liver tumors who cannot have surgery.
The reason we are able to do this is because the liver has two blood supplies: the hepatic artery and portal vein. Most liver tumors derive their blood supply from the hepatic artery and the natural pathway to tumor cells bypasses normal liver cells. In addition, the majority of normal liver is supplied by the portal vein and is mostly spared.


Cincinnati Children’s is one of the only pediatric hospitals to offer SIRT, and I am one of a few dedicated pediatric interventional radiologists who is an authorized user for yttrium-90, the radioactive agent used for SIRT. SIRT has been used extensively in adults to treat liver tumors, and here at Cincinnati Children’s we have treated 8 children with promising results. SIRT has been shown to provide palliative (pain reprieve) therapy, improve survival, and provide symptomatic relief.
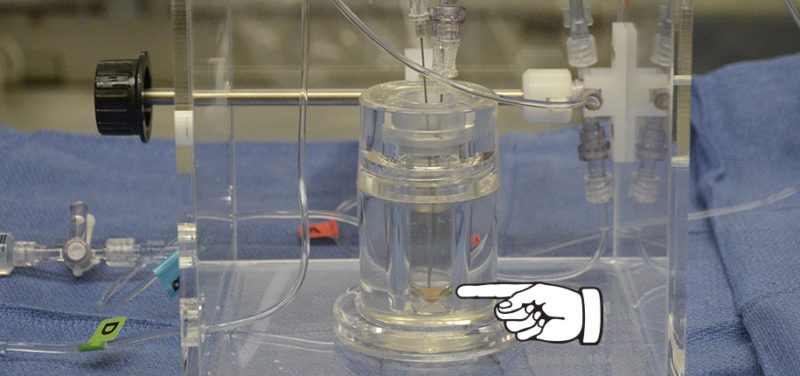 Photo: Close-up of container holding radioactive agent. Finger points to radioactive agent, on bottom.
Photo: Close-up of container holding radioactive agent. Finger points to radioactive agent, on bottom.
Contributed by Dr. Allison Aguado and edited by Tony Dandino, (RT-MRI).
