Magnetic resonance imaging (MRI) is an imaging method that uses the protons of hydrogen atoms within the body to generate a medical image. MRI of the lungs has historically been challenging for a few different reasons. One reason is that the proton signal of the lungs fades away a lot quicker in the lungs than in soft tissues (like muscle or liver), which means that the MRI equipment has to work very quickly to acquire the signal before it’s gone. Recent developments on “ultrashort” MRI techniques have greatly improved MRI visualization of the lungs, with some studies already using ultrashort MRI in adults and older children. However, our group’s study represents the first time anyone has used the ultrashort MRI with an infant population.
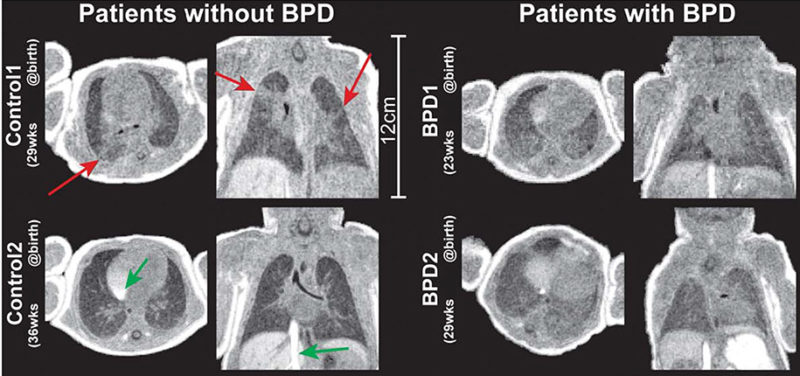
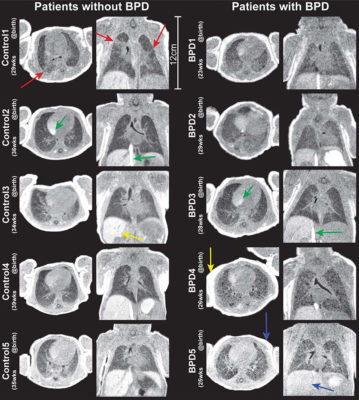 Figure: Views in the axial and coronal planes from 3D UTE image volumes. Patients with no clinical diagnoses of pulmonary disease (left column) are shown alongside patients diagnosed with BPD (right column). Red arrows highlight regions of distinctly heterogeneous parenchymal signal for Control1, a possible indication of subclinical pathology potentially linked to the prematurity of birth. Yellow arrows in Control3 and BPD4 highlight the bright liver and fat signal, respectively, associated with heavy T1 weighting obtained with the use of higher flip angles (8–108). Blue arrows show reduced contrast between muscle and both fat and liver in BPD5, due to the lower flip angle used (58 vs. 8–108). Green arrows highlight inflow effects in the right atrium and inferior vena
Figure: Views in the axial and coronal planes from 3D UTE image volumes. Patients with no clinical diagnoses of pulmonary disease (left column) are shown alongside patients diagnosed with BPD (right column). Red arrows highlight regions of distinctly heterogeneous parenchymal signal for Control1, a possible indication of subclinical pathology potentially linked to the prematurity of birth. Yellow arrows in Control3 and BPD4 highlight the bright liver and fat signal, respectively, associated with heavy T1 weighting obtained with the use of higher flip angles (8–108). Blue arrows show reduced contrast between muscle and both fat and liver in BPD5, due to the lower flip angle used (58 vs. 8–108). Green arrows highlight inflow effects in the right atrium and inferior vena
cava.
Premature infants can greatly benefit from lung imaging. The lungs are one of the last organs to develop in a fetus, and so a premature baby’s lungs aren’t quite ready yet to function and so have a lot of issues working normally. Sometimes X-ray radiographs and X-ray computed tomography (CT) are used to look at these babies’ pathological lung structures, but there are concerns about ionizing radiation exposure to infants over repeated imaging. Since MRI is non-ionizing, we decided to show that it is possible to use our ultrashort MRI techniques to image neonates with pulmonary issues.
In addition, we performed our neonatal lung ultrashort MRI study using a unique, infant-sized scanner that is located directly within the neonatal intensive care unit (NICU) of Cincinnati Children’s. The hospital’s other MRI scanners are located several floors away from the NICU, presenting logistical and medical challenges when bringing the babies away from their unit. The proximity of our NICU scanner to the babies’ beds makes it much easier and less risky to image them. As well, the small size of the scanner allows us to get much higher quality images of the infants when compared to conventional MRI scanners, which are big enough to fit an adult.
 Figure: a: The MRI scanner located within the CCHMC NICU, with a baby doll placed on the patient table, for reference. b: The pulse sequence diagram for the UTE sequence. The dotted line indicates the nutation point of the RF pulse, and the area of the pink shaded region is equal to zero at TE, represented by the star (at k-space center). c: Ten consecutive center-out radial kspace trajectories are shown, highlighting the pseudorandom view ordering and the repeated sampling of the k-space center, indicated again by a star. d: A 200-sec segment of the phase sampled from the center of k-space during an infant exam, with an example of bulk motion highlighted.
Figure: a: The MRI scanner located within the CCHMC NICU, with a baby doll placed on the patient table, for reference. b: The pulse sequence diagram for the UTE sequence. The dotted line indicates the nutation point of the RF pulse, and the area of the pink shaded region is equal to zero at TE, represented by the star (at k-space center). c: Ten consecutive center-out radial kspace trajectories are shown, highlighting the pseudorandom view ordering and the repeated sampling of the k-space center, indicated again by a star. d: A 200-sec segment of the phase sampled from the center of k-space during an infant exam, with an example of bulk motion highlighted.
Pulmonary MRI of Neonates in the Intensive Care Unit Using 3D Ultrashort Echo Time and a Small Footprint MRI System
Andrew D. Hahn, PhD, Nara S. Higano, MS, Laura L. Walkup, PhD, Robert P. Thomen, PhD, Xuefeng Cao, MS, Stephanie L. Merhar, MD, MS, Jean A. Tkach, PhD, Jason C. Woods, PhD, and Sean B. Fain, PhD
Read the full research article (click here).
Contributions by Nara Higano (Graduate Student , IRC) and edited by Glenn Miñano, BFA.