Prematurely born babies often have difficulty breathing on their own because their lungs have not fully developed before birth. Some of these babies require long durations of oxygen support or mechanical ventilation and are given a clinical diagnosis of bronchopulmonary dysplasia (BPD); however, the underlying lung structural pathology giving rise to BPD has not been well characterized. Using a small footprint magnetic resonance imaging (MRI) scanner located within the neonatal intensive care unit (NICU) at Cincinnati Children’s, we performed MR imaging in a small group of NICU patients to characterize BPD and the lungs of premature infants. This MRI scanner is unique because it’s sized for neonates (only an arm or leg of an adult would fit in this scanner!) and it’s located right in the NICU so the babies don’t have to go far for imaging. Cincinnati Children’s is the only institution in the United States to have a MRI scanner in the NICU.
 Image: MRI NICU scanner
Image: MRI NICU scanner
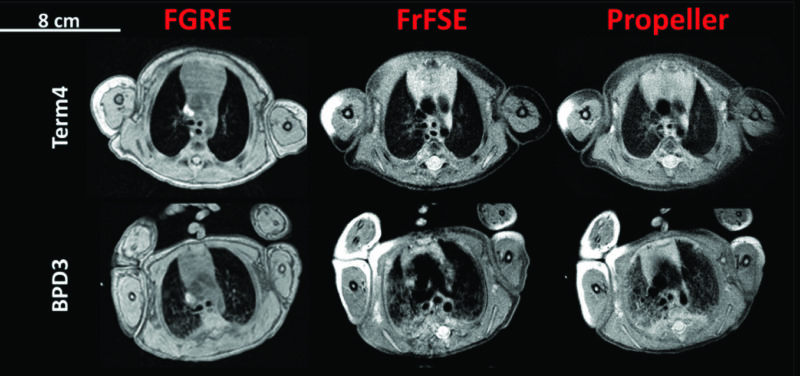
We imaged babies born at full-term, those born prematurely but without diagnosed BPD, and patients with BPD, and we found stark, measurable differences in the lungs between these groups. In particular, babies with diagnosed BPD had a larger amount of high-signal intensity lung tissue than other groups. Importantly, there was much variation in the appearance of the lungs across different BPD patients; some had more fibrosis while other patients had more hyperinflated lung tissue. This research suggests that there may be different types of BPD, and with future research, MRI may be used to assess individual NICU patients, monitor their lung growth and clinical progress, and eventually, be used to inform clinical-care decisions that improve outcomes.
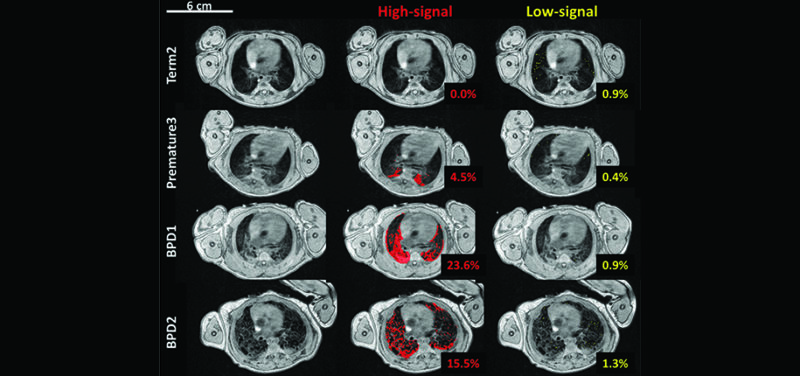 Image: Fast gradient echo image segmentation of high- and low-signal intensity parenchyma in four neonatal intensive care unit patients (top to bottom): a full-term control subject (Term2), a premature patient (Premature3), and two bronchopulmonary dysplasia (BPD) patients (BPD1 and BPD2). The first column is a representative axial slice near the hilum without masking. High-signal (defined as pixels .45% of the mean chest soft tissue signal) and low-signal (.4% of the mean chest soft tissue signal) lung parenchyma are indicated in red and yellow, middle and right columns, respectively. The volume percentages of the thresholded pixels for the whole-lung analysis are included.
Image: Fast gradient echo image segmentation of high- and low-signal intensity parenchyma in four neonatal intensive care unit patients (top to bottom): a full-term control subject (Term2), a premature patient (Premature3), and two bronchopulmonary dysplasia (BPD) patients (BPD1 and BPD2). The first column is a representative axial slice near the hilum without masking. High-signal (defined as pixels .45% of the mean chest soft tissue signal) and low-signal (.4% of the mean chest soft tissue signal) lung parenchyma are indicated in red and yellow, middle and right columns, respectively. The volume percentages of the thresholded pixels for the whole-lung analysis are included.
LL Walkup, et al. Quantitative magnetic resonance imaging of bronchopulmonary dysplasia in the NICU environment.
Laura L. Walkup, Jean A. Tkach, Nara S. Higano, Robert P. Thomen, Sean B. Fain, Stephanie L. Merhar,
Robert J. Fleck, Raouf S. Amin, and Jason C. Woods
*This article was featured by Pulmonary Medicine in the 2016 Research Discoveries publication. Read the full research article (click here).
Contributions by Nara Higano (Graduate Student , IRC) and edited by Glenn Miñano, BFA.